Obstetrics & Gynaecology final exam experience
I'm back!!! I know I took a little bit longer of a hiatus from my blog than I said I would, but since returning to Pécs, all I have been doing is studying and preparing for my exams. Today, I successfully completed my Obstetrics and Gynaecology final exam, and I want to share my experience with you.
The exam was scheduled to start at 8 am this morning. All the students were there, but this did not happen. At around 8:30 am, someone finally showed up and welcomed all the English Program students into the large lecture room. One by one, we were able to choose our four topics. I pulled the following,
2. Ovarian Cancer: Classification, symptoms and diagnosis
3. Diabetes and Pregnancy (Screening and Management)
4. Maternal Obstetrical Injuries
I grabbed some paper and sat down to write out my topics until the doctor came to examine us. The examiner was Dr Tamás.
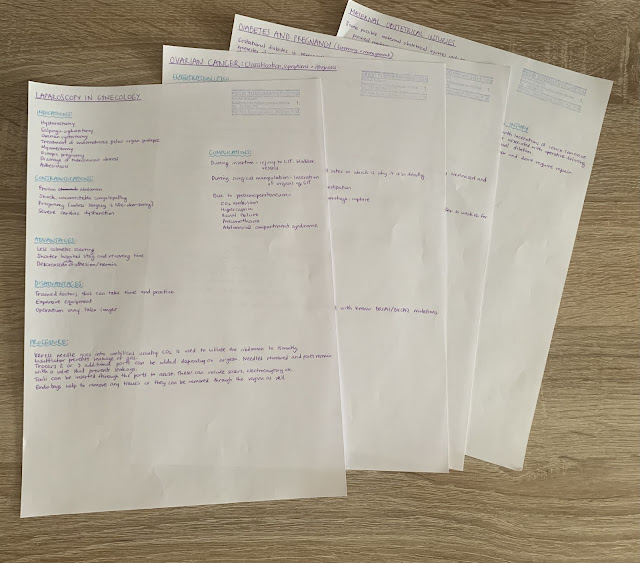 |
These are what my notes from the exam look like. |
I am not sure how much time passed, but when the doctor arrived I was just beginning to write my fourth topic. Another student was ready with her topics and started her exam, while the rest of us continued writing. Two more students had their exams, then it was my turn.
Now came the hard part, to present my topics. I began with the Laparoscopy in Gynaecology topic,
Doctor: What is laparoscopy?
Me: It is an operation where you do not cut open the whole abdomen but rather use small incisions with a camera and other ports to see inside.
Doctor: Tell me about the steps of the procedure.
Me: You insert the Veress needle into the umbilicus and insufflate the abdomen with CO2 until 15mmHg. Once you have reached the desired pressure, the needle is removed and replaced with an insufflator. The insufflator maintains the pressure inside the abdomen and prevents leakage of the gas. At this point, the patient is put in the Trendelenburg position. Incisions are made on the lower abdomen for other ports. To prevent injury to any vessels, the camera light is used when making the incisions. Sometimes two additional ports are used, sometimes three. It is up to the surgeon.
Doctor: Good, what are some indications for laparoscopy?
Me: Hysterectomy, salpingo-oophorectomy, treatment of endometriosis, ovarian cystectomy, ectopic pregnancy, adhesiolysis, drainage of tube-ovarian abscess...
Doctor: Next topic…
Next, I talked about the Ovarian Cancer topic. I explained the FIGO classification as written on my paper, described the symptoms and diagnosis of ovarian cancer. When I finished speaking about what I had written, the doctor had some questions,
Doctor: If a mother has ovarian cancer, what do you do for the daughter?
Me: Check for BRCA1/2 gene mutations.
Doctor: Yes, we do genetic testing, and if it’s positive?
Me: If the daughter is within childbearing age and would like to have children, do annual ultrasound examinations. However, if the daughter is older than childbearing age or does not want to have any children, do a total hysterectomy with bilateral salpingo-oophorectomy.
Doctor: Yes, radical oophorectomy (looks at the topic) I think the classification here was meant to be histological not FIGO.
Me: Oh, really?
Doctor: Yes, like epithelial, germ cell...
Me: Well, for epithelial tumours it can be mucinous, serous, clear cell, or endometrioid types. For germ cell tumours it can be teratoma, dysgerminoma...Then, there are sex-cord stromal tumours...
Doctor: That's good, next topic.
Next, I did the Diabetes and Pregnancy topic. I started by explaining the definition of Gestational Diabetes and Pre-gestational Diabetes. I mentioned the risk factors, then the doctor interrupted,
Doctor: When do we do screening?
Me: Screening is normally done in weeks 24-28, but in high-risk populations, it is done in week 16.
Doctor: Okay, so now we have done the screening and know the patient has diabetes, the woman is 36 weeks, what do we recommend?
Me: Lifestyle changes. Particularly, restricted diet to 180g carbohydrates per day.
Doctor: And then, if that doesn't work?
Me: Next, would be insulin therapy and continuous monitoring of the foetus.
Doctor: Last topic...
I finished with the Maternal obstetrical injuries.
Me: The most common maternal obstetrical injury is perineal rupture. There are 4 degrees of perineal rupture...Treatment is with surgical repair and DRE should be performed after.
Doctor: What is an internal injury that might not be seen?
Me: Cervical injury.
Doctor: Well, that can be seen.
Me: Retroperitoneal haematoma.
Doctor: Rupture of what muscle causes retroperitoneal haematoma?
Me: Uterus?
Doctor: The levator ani.
I was done with my topics and thought this was where my exam would end but the doctor had other plans.
Doctor: It's between a 4 and 5. I am going to ask you a question for a 5.
I nodded.
Doctor: What is the mechanism of action of vasodilation in early pregnancy?
Me: Progesterone.
Doctor: And? Think paracrine hormones.
Me: I am not sure.
Doctor: Okay, it’s a 4. Do you want to know the answer?
Me: Yes, please.
Doctor: N2O, H2S, CO2, Prostacyclin.
Me: Thank you.
Doctor: I’m really sorry, you had the best knowledge today. I hope we will meet again at the final exam.
That's one down, five more to go.




Comments
Post a Comment